Call to book or for more information 01444 410944
Running injuries
Going the extra mile: The most common running injuries, their causes, symptoms and how to help yourself (Part 1)
Written by Chris Brooks. Osteopath at The Perrymount Clinic
Marathon season is well and truly upon us and so now is as good a time as any to review the most common running injuries and best course of action for their management. Of course, this isn't just aimed at those of you who will endeavour to run 26.2 miles in the coming days and months, it is also relevant for anyone trying to lose weight or tone up after a long winter.
Whatever the reason behind an increase in physical activity, running is the backbone of many people’s exercise regime but this ramping up of miles on the body’s odometer does not usually happen without some tweaks, sprains and strains along the way. This is the first part of my guide to the most common running injuries that present themselves here at the Perrymount Clinic. Let’s work from the back down to and including the knee in this first instalment.

Non-specific lower back pain in runners
Location of the pain:
The lower back.
Symptoms:
A pain and/or stiffness in the lower back that often comes on after running for 10 minutes. The pain may refer into the buttock, but does not extend below the knee and there is no no pins and needles or numbness in the legs. Pain is generally worse for bending backwards or sideways, although simple tasks such as putting your shoes on may be uncomfortable. Stiffness and a sense of vulnerability can also be felt at times when not running.

The detail:
Non-specific lower back pain is a diagnosis that is frequently given for people with lower back pain when the precise tissue causing the pain is not known. The facet joints of the spine, the intrinsic spinal ligaments and muscles, the large paraspinal muscles, as well as the sacroiliac joints, may be implicated.
In runners we often see a similar problem. After all, runners often complain lower back pain is stopping them from running, but they don’t see it as an injury caused by running, like they would a muscle strain or ligament sprain in the leg. However, this is misguided, because if you accept your back pain is a running injury, you can make adjustments to your running style, duration and frequency that will be an important step towards curing your back pain.
Self-management:
Ice the area - there is likely to be inflammation and irritation of the facet joints.
Attend to your core strength - the muscles that surround the lower back are frequently neglected by runners. These muscles act as a corset of sorts and provide increased stability for the lower back.
Attend to any other niggles in the legs you may have - these could be causing you to compensate through your pelvis and lower back.
Reduce hill running - the downhill sections will bring the joints of the spine closer together.
Use a foam roller or tennis ball to work on the myofascial trigger points (hyper-irritable spots in the fascia surrounding skeletal muscle) of the muscles on each side of your spine.
Gluteus medius tendinopathy
Location of the pain:
Hip and gluteal muscles (buttocks)
Symptoms:
Commonly an aching pain and stiffness around the outer hip. Often there will be no discomfort in the early stages, but the pain will increase with the length of the run. Other symptoms may include: inflammation, heat or redness of the local area, pain and stiffness when first waking, tenderness of the immediate area.
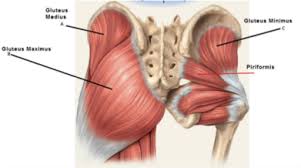
The detail:
Gluteus medius tendinopathy is commonly an overuse injury rather than a result of direct trauma. The tendon of this muscle attaches to the hip bone, and like all tendons it is a rough fibrous tissue and therefore when subjected to repetitive actions (such as running long distances) it can develop micro tears that have difficulty fully recovering without an adequate healing period.
Self-management:
Ice the local area after a run.
Space out runs to give the tendon time to recover. Better still, rest from running completely until symptoms reduce substantially.
Sit on a tennis ball, with the ball under your buttock muscle (you can use a harder ball of similar size, but it will hurt more) to give yourself a trigger point massage.
Hamstring tendinopathy
Location of the pain:
On and just below the ‘sitting bone’ of the lower buttock.
Symptoms:
Commonly an aching pain and stiffness around the outer hip. Often there will be no discomfort in the early stages, but the pain will increase with the length of the run. Other symptoms may include: inflammation, heat or redness of the local area, pain and stiffness when first waking, tenderness of the immediate area.
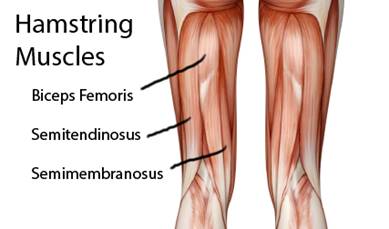
The detail:
The hamstring group is comprised of three muscles. They attach to the leg bones beyond the knee and span the length of the thigh attaching to ischial tuberosity, often know as the ‘sitting bone’. When the hamstrings become overused and thus overstressed it is often the tendon or the musculotendinous junction that suffers from micro tears or strains. This is particularly seen where there has been a quick increase in intensity or length of activity.
Tendon strains will cause localised pain and inflammation and should not be ignored. They are a symptom of an overuse injury and unless appropriate action is taken the tendinopathy will become a chronic problem and will be far harder to rectify.
Self-management:
Ice the area in the early stages of the injury - place the ice on and just under the ‘sitting bone’.
Use trigger point massage and foam-rolling to decrease the muscular tone of the hamstrings.
Avoid using the classic method of stretching the hamstrings (leg straight and bending forward) as this will just create further stress on the tendinous attachment.
Iliotibial band syndrome
Location of the pain:
Outer side of the knee.
Symptoms:
Pain on the outside of the knee that increases with persistent bending and straightening of the joint. There may even be popping or snapping from the outer knee. This is often noticeably worse with heel strike. There may be localised swelling and redness.
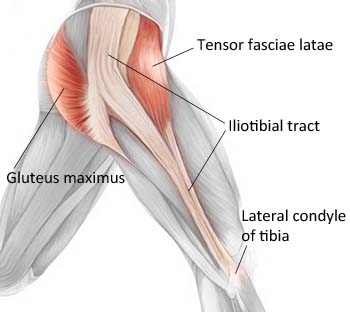
The detail:
The iliotibial band, often called the IT band, runs from the area of your hip to the fibula bone in the lower leg. It is made up of extremely strong tissue and its purpose is to stabilise the knee throughout its whole range of motion. However it can with increased activity friction against the protuberance on the outer edge of the femur (thigh bone). This can result in localised inflammation and pain.
Self-management:
Apply ice to the local area to manage inflammation.
Use a foam roller on the outer thigh in order to target the IT band itself as well as adjoining muscle groups; quadriceps, hamstrings and gluteals.
Rest the problem and manage it before it becomes chronic and persistent.
Patellofemoral pain syndrome (knee)
Location of the pain:
Below and around the kneecap
Symptoms:
Discomfort and tightness around or deep to your patella (kneecap). It can also be felt as a sharp pain. Discomfort often disappears quickly with lack of movement of the knee (although the tightness may remain). Symptoms may be more obvious when running uphill, going up and down stairs and when sitting for long periods. There may be an increase in grinding of the patella.
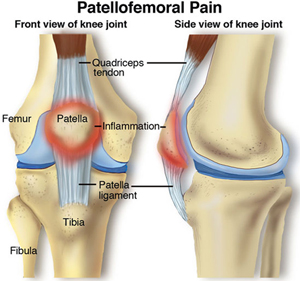
The detail:
In a healthy knee the patella moves smoothly with relative contraction and relaxation of the large quadricep muscles. With patellofemoral pain syndrome, or ‘runner’s knee’ the patella can move inappropriately with a deviation towards the outer knee. This is thought to be due to a muscular imbalance of the large quadriceps muscles. The upshot is irritation and damage to tissues beneath and local to the patella.
Self-management:
Due to the fact that muscular imbalances within the thigh muscles are a causative factor it is important to reduce tone in vastus lateralis (outer front thigh muscle) with liberal foam rolling and stretching.
Equally vastus medialis and vastus medialis obliqus (inner front thigh muscles) should be strengthened with appropriate exercises to counteract vastus lateralis.
Taping of the knee can be introduced to encourage patella alignment.
If your symptoms seem to match any of the above injuries, try to apply some of these common-sense self-management techniques. The list is far from exhaustive, but gives an idea of what we see at the Perrymount Clinic more frequently. Why not call for an appointment and we can take a look at the problem and advise you on an individual basis as to the best treatment and management approach for you. In this way we could save you a great deal of pain and time away from running.
In the next instalment, I will look at common running injuries below the knee.
Going the extra mile: The most common running injuries, their causes, symptoms and how to help yourself (Part 2)
Shin Splints
Location of the pain:
Along the inside of the shin.
Symptoms:
Recurring pain in the middle and inner aspect of the tibia (shin bone). Often described as an aching or a sensation of increasing pressure that intensifies until the pain forces the person to cease activity.

The detail:
In summary, it is the inflammation of the connective tissues joining the muscle to the inside of the tibia. It is caused by overuse or too sudden increased activity levels. Running on surfaces that are hard and/or an upwards gradient probably can also contribute.
Self-management:
Use ice to decrease localised inflammation.
As hard as it will be for you really keen runners, it may be necessary to stop running for a prolonged period. You can of course maintain cardiovascular fitness by diversifying into non-weight-bearing exercise, such as cycling or swimming.
Consider foot and gait analysis to see if there is an underlying predisposing factor such as dropped medial arches of the foot and resultant tibial torsion.
Achilles tendonitis
Location of the pain:
In the Achilles tendon itself, but also felt in the back of the heel where the tendon attaches.
Symptoms:
An ache in the Achilles tendon that is often made worse with activity. Continuing to run through the discomfort can make the micro-tears associated with tendonitis worse and result in a longer recuperation period. The injury may also cause redness or swelling around the tendon and a sensation of tightness within the lower calf. Where there is a palpable lump within the tendon or an audible snapping sound, this may be due to a build-up of scar tissue due to a longer period of successive micro trauma.
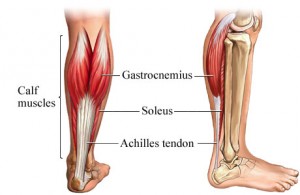
The detail:
The Achilles tendon is what connects your calf musculature to your heel. It is the biggest tendon in your body, and it needs to be, as it has to deal with large forces when walking, let alone running or jumping. The problem will often begin as a mild ache in the area after sporting activity. Prompt action can reduce the length of time needed to rehabilitate the area. Many factors are thought to predispose someone to Achilles tendonitis, including an increase in the intensity of activity, poor running technique, inappropriate footwear.
Self-management:
Ice the area, especially after activity.
A small heel lift may be helpful in reducing discomfort in the tendon itself – the lift slightly shortens the calf musculature and so reduces pull and stretch on the Achilles.
Plantar fasciitis
Location of the pain:
Underside of the foot
Symptoms:
Tenderness, stiffness or even a sensation of bruising in the sole of the foot. It often begins around the base of the heel. Stiffness in particular may be more evident upon weight-bearing for the first steps of the day or after a period of inactivity. Discomfort is also more likely when barefoot or wearing unsupportive footwear.
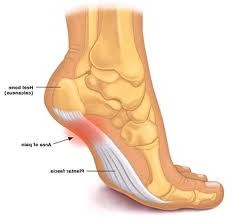
The detail:
The plantar fascia is an extremely strong band of connective tissue that supports your foot arches. Its main purpose is to absorb much of the impact of heel strike and help to reform the foot arches after toe-off. With micro-tears in the fascia we get discomfort. Some people appear to be more prone to this and it is likely that there are several predisposing factors such as increased weight, inappropriate footwear, lack of stretching and increased activity.
Self-management:
- It is possible to continue running through the discomfort for a prolonged period, but doing so will cause an exponential increase in healing time.
- While applying a moderate amount of pressure, roll the sole of the foot over a rolling pin for around five minutes a time, up to five times a day. This can also be done with a frozen water bottle if you wish to combine the benefits of icing with the facial stretch.
- Stop wearing any non-supportive footwear such as flip flops, sandals, etc.
- Liberal foam rolling of the calves and stretching of the calf muscles can be of benefit when suffering from plantar fasciitis.
Ankle ligament sprain
Location of the pain:
On the side of the ankle
Symptoms:
Swelling, bruising, instability, pain and difficulty weight-bearing fully on the affected side, depending on the severity of the sprain. Often it may just be mildly uncomfortable with residual stiffness. However, when severe, all the above symptoms will present themselves in the days following the injury. It is also worth noting that pain, swelling and inability to weight-bear can be a sign of a fracture, so if you are worried you should visit A&E as soon as possible.
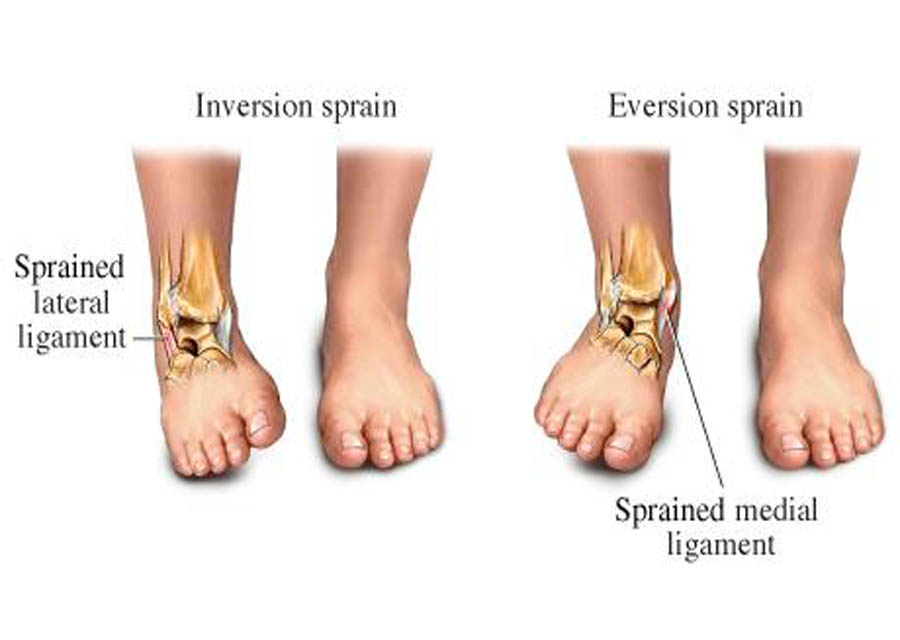
The detail:
Inversion strains (when you roll on to the outside of your foot) are fairly common. Most people have experienced this to some extent, perhaps after losing their footing in a pothole, or during sporting activity where they have had to change direction quickly. Severity can range from a mild tear to a complete rupture.
Self-management:
- Rest
- Ice the area regularly – for up to 10 minutes at a time.
- Compression bandages can help with the initial swelling.
- Elevate the ankle from time to time to aid with the reduction of swelling.
- Once the initial discomfort and swelling have reduced, proprioceptive exercises that help your body control the movement of your ankle can be undertaken in order to decrease the likelihood of further sprains.
Print out this voucher for a £10 discount off an osteopathy treatment with Chris at The Perrymount.
If you would like to book an appoinment with one of our osteopaths please give us a call on 01444 410944 or leave us a few details below and we will be in touch with you shortly
Feel free to download any of our self-help and educational e-books, just click the link below


Sign up to our newsletter for 6 free health ebooks and £100 of treatment vouchers
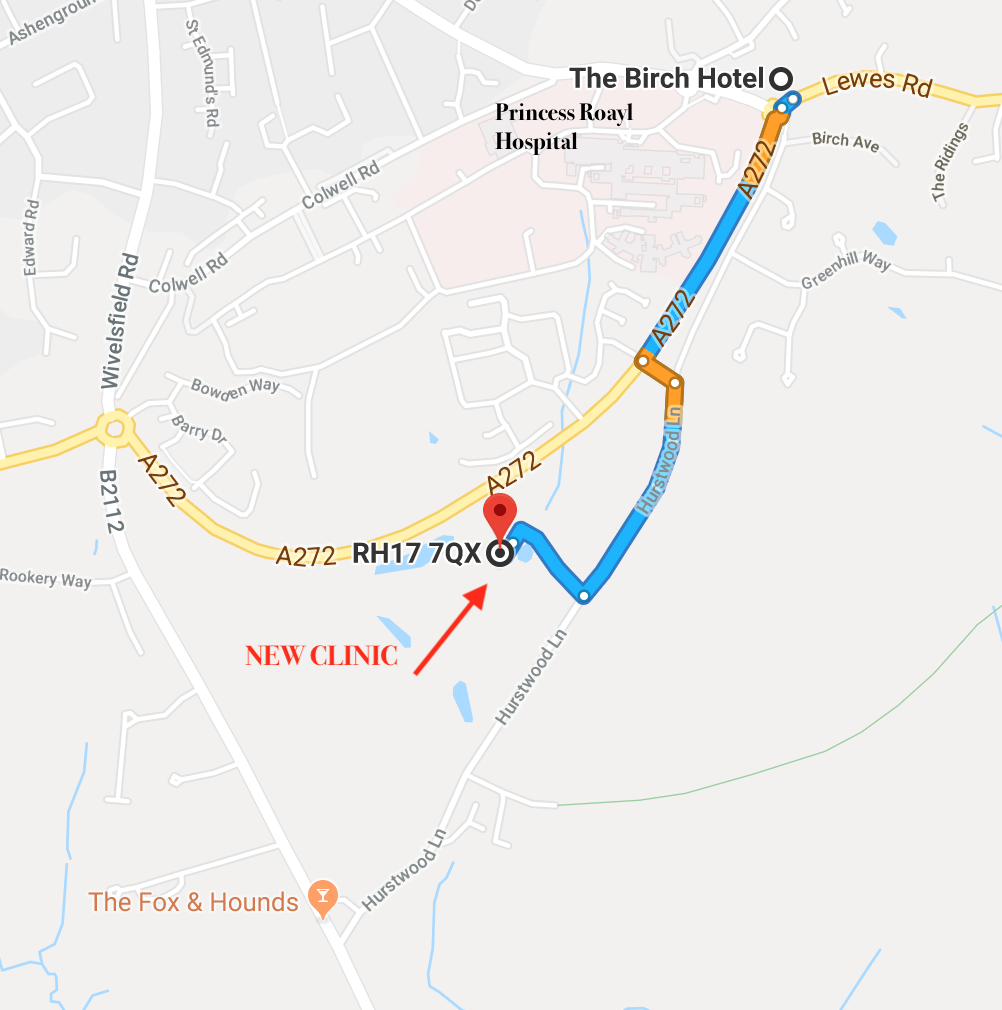
The Perrymount Clinic
Unit 5
Hurstwood Grange
Hurstwood Lane
Haywards Heath
West Sussex
RH17 7QX
01444 410944
info@theperrymount.com




